More Information
Submitted: September 27, 2024 | Approved: October 03, 2024 | Published: October 04, 2024
How to cite this article: Chase H, Lauren H, Jonathan I, Sydney K, Johnny C. Proactive Psychiatric Consultation and Hospital Length of Stay in Adults: A Review of the Literature. Arch Psychiatr Ment Health. 2024; 8(1): 041-046. Available from: https://dx.doi.org/10.29328/journal.apmh.1001056
DOI: 10.29328/journal.apmh.1001056
Copyright License: © 2024 Chase H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Proactive consultation-liaison psychiatry; Psychiatric disorders; Hospital Length of Stay (LOS); Mental health; Psychiatric services
Proactive Psychiatric Consultation and Hospital Length of Stay in Adults: A Review of the Literature
Hathaway Chase, Haley Lauren, Irby Jonathan, Klumb Sydney and Cheng Johnny*
College of Osteopathic Medicine, Rocky Vista University, USA
*Address for Correspondence: Cheng Johnny, College of Osteopathic Medicine, Rocky Vista University, USA, Email: [email protected]
According to a 2022 systematic review on the prevalence of psychiatric disorders in general hospitals, it was estimated that approximately one-third of medical inpatients present with a coinciding psychiatric condition. However, other studies have reported that a low rate of patients actually obtain an inpatient psychiatric consult; and even fewer patients receive a consultation when it would not be traditionally indicated. Therefore, we have seen an emergence of the use of Proactive Consultation-Liaison (C-L) Psychiatry across many hospital settings. This model of care utilizes systematic screening for active mental health concerns, proactive interventions tailored to individual patients, team-based delivery, and care integration with primary services to provide psychiatric consultation earlier. This study conducted a focused PubMed search to review the research to date on proactive C-L psychiatry and its impact on hospital length of stay (LOS) in patients over 18 years old. Results show a consequential reduction in average hospital LOS when proactive C-L psychiatry services are used compared to reactive, on-request consultation services. A shortened LOS is seen with this practice when there is a quicker time for consultation or referral. Thus, there is evidence of proactive C-L psychiatry’s success in decreasing average hospital LOS and improving patient care. Additional studies are necessary to determine its significance, as little research to date has been completed on the topic. It is recommended to expand the scope of investigation to different patient populations, including but not limited to pediatrics and patients without an underlying mental health illness.
According to a 2022 systematic review on the prevalence of psychiatric disorders in the general hospital setting, it was estimated that approximately one-third of medical inpatients present with a coinciding psychiatric condition [1]. Thus, it is evident that a noteworthy amount of patients may require psychiatric attention while hospitalized. However, other studies have reported that a low rate of patients actually obtain an inpatient psychiatric consult when in the hospital. Additionally, even fewer patients receive a consultation when they do not have an identified psychiatric illness or when it would not be traditionally indicated. A study in 2006 used the Clinical Interview Schedule (CIS) assessment to categorize patients needing mental health care. They found that 5% of patients not requiring a consultation had one performed, while only 33.3% of inpatients needing a psychiatric consultation actually obtained one [2]. Another observational study completed in 2018 revealed that under 1% of patients without a behavioral health condition had a psychiatric consultation conducted, and only 14.5% of patients with an underlying mental illness received a consultation [3]. Therefore, it is clear that the rate of inpatient psychiatric consultation is low— no matter if the patient has an underlying mental health condition or not.
Research stresses the importance of providing psychiatric consultations in a proactive manner, not only to improve the care for those identified in the hospital as having a psychiatric illness but also for those who are not. As a result, we have seen a shift in the standard of care of consultation psychiatry with an aim of delivering mental health care to a wider range of patients. In 2019, the Proactive Consultation-Liaison (C-L) Psychiatry Special Interest Group (SIG) was created through the Academy of Consultation-Liaison Psychiatry, as a direct result of studies and data that showed proactive C-L psychiatry’s impact on healthcare. A resource document on the consultation strategy was drafted in July 2020 by this SIG and finalized later in 2020. The document outlines the history and developments of C-L psychiatry that ultimately formed the current goals of care of the proactive model used today. These include systematic screening for active mental health concerns, proactive interventions tailored to individual patients, team-based care delivery, and care integration with primary teams and services. As seen in Table 1, the components of proactive C-L care have adapted from traditional C-L psychiatry via empirically derived strategies that were created to best suit the changes in psychiatric patient needs in medicine today [4].
| Table 1: Application of empirically derived strategies in C-L. | ||
| Elements of traditional C-L | Empirically derived strategy | Elements of proactive C-L |
| Many psychiatric needs go inidentified | Population approach | Systematic screening for active mental health concerns |
| Mental health care tends to be crisis-focused | Prevention mindset | Proactive clinical intervention tailored to clinically relevant needs |
| Recommendations and support chiefly to clinicians | Multidisciplinary teamwork | Interdisciplinary team-based approach that addresses the unique needs of patients |
| Liaison role variable, based on setting, service, or population | Cross-specialty integration | Real-time integrated care delivery through clinical partnership with primary teams |
| C-L = Consultation-Liaison. Note: Use of empirically derived strategies (center column) to form the goals of the current proactive C-L model (rightmost column) from the traditional model (leftmost column). |
||
Studies have found many positive outcomes related to proactive C-L psychiatry, including reduced time to consultation, increased provider satisfaction, and decreased hospital length of stay (LOS). It is these findings that have encouraged further use of proactive C-L psychiatry among different hospital settings and patient populations. These advancements in care are not just applicable to patients but to physicians, nurses, other healthcare staff, and hospital teams and systems as a whole. To achieve the best understanding of the proactive C-L psychiatry model used today, it is crucial to appreciate the team members and their roles (Table 2) [4]. Coordinated care is needed in order to provide the best outcomes, and each member of the proactive C-L team plays an equally important part in delivering that care.
| Table 2: Proactive C-L psychiatry team members. | |
| Team member | Roles |
| Attending psychiatrist | Medical director |
| • Oversees clinical care and supervises daily rounds | |
| • Coordinates with primary service leadership | |
| • Performs formal consultations | |
| • Assumes medicolegal responsibilities such as psychiatric commitments or capacity assessments (as per local jurisdiction and hospital policy) | |
| • Supervises consults performed by trainees (as needed) | |
| Psychiatric nurse practitioner | Primary point of contact for primary teams |
| • Triages consultations | |
| • Oversees daily care workflow | |
| • Leads the development of nursing behavioral care plans | |
| • Performs formal consultations | |
| • Assists with screening process | |
| Clinical social worker | Team coordinator |
| • Collaborates with social worker and care manager on the primary service | |
| • Routinely evaluates patients with psychiatrist or nurse practitioner | |
| • Works with families, community resources, and other collateral data sources | |
| • Coordinates mental health aftercare | |
| • Assists with screening process | |
| Clinical nurse specialist (optional) | Behavioral and systems specialist |
| • Creates tailored behavioral care plans | |
| • Provides hands-on training to nurses to manage challenging behaviors (e.g., modeling de-escalation, suggesting environmental approaches) | |
| • Identifies system-level contributors to care inefficiencies | |
| • May provide care recommendations based on training and expertise | |
| • May contribute to hospital policies on behavioral management | |
| Service administrator (optional) | Team administrator |
| • Reviews administrative team needs in collaboration with medical director | |
| • Supports healthy team dynamics | |
| • Organizes regular team meetings for institutional or other updates relevant to team functioning | |
| • Helps to align team priorities with institutional missions | |
| Clinical health psychologist (optional) | Psychological and behavioral specialist |
| • Performs clinical assessments, often in collaboration with other team members | |
| • May focus on specific populations or conditions (e.g., multimodal pain management, adjustment to medical illness, CBT modules, mindfulness) | |
| • May provide neuropsychological testing | |
| • May provide patient, family, and/or staff education | |
| Psychiatric and medical trainees (optional) | Medical students, residents, or consultation-liaison psychiatry fellows |
| • Roles as assigned by the training program curriculum | |
| • Care supervised by attending psychiatrist | |
| C-L= Consultation-Liaison. Note: Proactive C-L team members (left column) with respective roles of each member (right column). |
|
The purpose of this review is to investigate the literature on proactive C-L psychiatry and its associated impact on hospital LOS. The primary focus of this study is to determine the trend in average LOS among inpatients, in both general and ICU patient populations, who receive proactive C-L psychiatry.
Contributing topics include time to referral or consultation, healthcare staff satisfaction, and subsequent rate of readmission. The results of the studies addressing these topics are discussed in their respective sub-headings, done so in a chronological manner in order to acquire a better understanding of the above relationship and how it has changed over time.
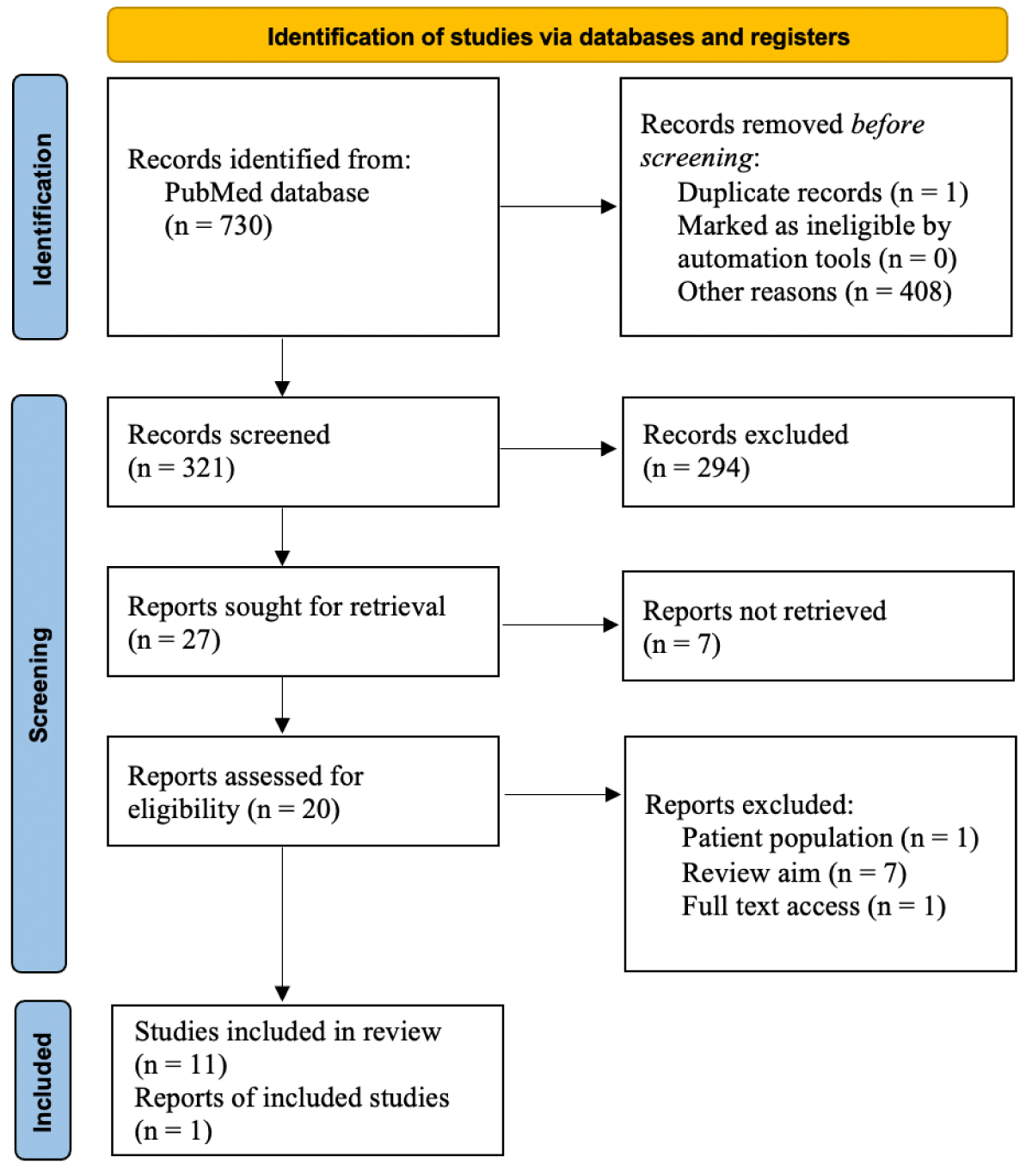
A search was conducted on PubMed, starting with the keywords (“psychiatric consultation”) AND (“hospital length of stay”), which yielded 730 total articles. From here, inclusion and exclusion criteria were utilized to narrow the search. Inclusion criteria were: (1) studies on proactive psychiatric consultation and LOS, and (2) adults over age 18. Keywords (“proactive psychiatric consultation”) AND (“hospital length of stay”) AND (“adults”) allowed for a focused search on articles better addressing the research question, which produced 20 different articles. Exclusion criteria were: (1) studies on the pediatric population under age 18, (2) articles that were not relevant to the aim of this literature review, and (3) articles without an available full text. 1 article was omitted for investigating the pediatric population, another 7 articles were omitted for lack of addressing the research question, and 1 article was omitted for not having accessible full text (Figure 1).
Figure 1: PRISMA flow diagram of included and excluded studies during the review process.
This resulted in 11 articles, spanning the last 14 years, to be included for review. Original sources cited in these articles were also reviewed and included as appropriate.
General inpatient hospital LOS
From the search, the first study that addresses hospital LOS with proactive C-L psychiatry was completed in 2011 by Desan, Zimbrean, Weinstein, et al. In this quasi-experimental trial, it was discovered that the intervention group that met with the staff-attending psychiatrist each weekday had an average LOS of 2.90 ± 2.12 days versus 3.82 ± 3.30 days in the control groups (χ2 = 6.38, df = 1, p = 0.01), and the fraction of cases with LOS > 4 days was significantly lower, 14.5% versus 27.9% (χ2 = 4.57, df = 1, p = 0.03) [5].
A study in 2015 by Sledge, Gueorguieva, Desan, et al. investigated the medical inpatient LOS among both non-ICU and ICU patients. Regarding the non-ICU patients, it was reported that the mean LOS in patients cared for by the proactive behavioral intervention team (BIT) was 5.84 ± 4.95 days, whereas patients that were being treated by the conventional consultation (CC) team had an average LOS of 6.38 ± 5.34 days (p = < 0.001) [6].
There were multiple studies completed in 2019 that addressed proactive C-L psychiatry and resultant hospital LOS. First, a study completed by Triplett, Carroll, Gerstenblith, et al. found that inpatients seen by the proactive consult team had a shorter LOS than the inpatients cared for by traditional consultation. Results revealed an LOS of 6.68 days for the proactively treated patients and an LOS of 8.54 days for the reactively treated patients (p = 0.005) [7]. Another study from 2019 by Oldham, Chanal, and Lee used a systematic review of 12 included studies to evaluate how many of these articles reported a reduced LOS with the proactive psychiatric consultation model— similar to the scope of this review. The authors found that 8 of these 12 articles to date had found a significant reduction in LOS. All 8 of these were studies in which the proactive C-L psychiatry was informed and screened by clinicians with a background in mental health care or primary psychiatric service [8]. A final study completed in the same year by Bronson, Alam, and Schwartz staffed a newly hired full-time attending in a small non-teaching general internal medicine unit to integrate the proactive C-L psychiatry model. Throughout the year, some patients obtained proactive interventional consultation while others received usual care. The results of their study revealed that the average LOS was 6.4 days (± 5.6) in the intervention group and 8.3 days (± 10.6) in the control group (p = 0.003) [9].
A data review in 2021 by Chavez, Caplan, McKnight, et al. looked at patient data from 2018 and found that proactive psychiatric consultation was associated with an average in-hospital length of stay that was 2.9 days shorter (± 1.3, 91% CI -5.36 to -0.45, p = 0.021) [10]. Another study completed in 2021 by Oldham, Lang, Hopkin, et al. investigated the Proactive Integration of Mental Health Care in Medicine (PRIME Medicine) model, which used proactive consults. It was launched in 2018 to serve 3 hospital medicine units at an 875-bed referral center and patients were followed throughout the year. They found that patients on PRIME units had an average LOS that was lower than the expected stay length by 2.5% (−0.16 d, p = 0.08). Mean LOS was observed at 6.44 days, compared to an expected 6.59 days; these results were not statistically significant. The authors did find, however, that PRIME Medicine led to increased rates of completed psychiatric consultation. The authors do note many limitations to this study, including the advanced age of the studied cohort and a large number of patients discharged to skilled nursing facilities [11]. These factors may have contributed to the results being statistically insignificant.
Lastly, there have been a couple of studies completed in 2024 to the point of this review’s conclusion. A study completed by Triplett, Prince, Bienvenu, et al. looked at EMR data over 4 years, from 2017 to 2021, which reflected the work of a Proactive Hospital-based Intervention to Provide Psychiatric Services (PHIPPS) team that was first implemented in 2016. They found the average LOS among proactive consultation service patients to be 7 days while the average LOS for on-request consultation service patients was 10 days (p = < 0.001). They do note that the on-request team was found to care for a sicker patient population, which could have contributed to these results [12]. In addition, Sharpe, Walker, van Niekerk, et al. reported the first randomized control trial on proactive C-L psychiatry in 2024. This study assessed the impact of Proactive Integrated Consultation-Liaison Psychiatry (PICLP) on medical inpatients over 65 years old between 2018 and 2020. The results revealed that PICLP patients had a mean LOS of 11.37 days (± 8.74) versus 11.85 days (± 9.00) with usual care (p = 0.18). Therefore, the difference in LOS among the treatment and control groups was not statistically significant. However, the study does report that the rate of discharge was 8.5% higher for PICLP patients (RR = 1.09, 95% CI 1-1.17, p = 0.042). The rate of discharge was especially increased when LOS was less than 14 days [13].
These studies show that proactive C-L psychiatry has resulted in a decreased mean LOS in the general inpatient population among all studies completed over the last two decades. The number of days reduced as a function of time cannot be obtained from this data, but the research has disclosed consistent findings of a reduction in hospital LOS with the use of the proactive service. The data is varied in regard to its statistical significance.
ICU patient hospital LOS
As noted above, the Sledge, Gueorguieva, Desan, et al. study in 2015 also investigated patients in the ICU setting. Among those receiving proactive behavioral intervention, the mean LOS was 9.41 ± 6.42 days. Among those who received conventional care, the mean LOS was 11.12 ± 7.30 days (p = < 0.001) [6]. A separate prospective cohort analysis done in 2019 by Bui, Thom, Hurwitz, et al. investigated two medical ICU (MICU) populations, the intervention of attaining daily psychiatric consultation, and the control of obtaining conventional consultation when considered necessary. Results showed a decrease in LOS in the hospital for the intervention patients at 6.92 days (interquartile range 3.70-14.31) versus 7.69 days (interquartile range 3.95-16.21) for the control group (p = 0.113). On the other hand, there was not a statistically significant reduced LOS in the MICU among these groups [14].
From these two studies it can be seen that reduced hospital LOS with proactive C-L psychiatry is applicable to the ICU patient population, not just the general hospital patient setting. However, there is mixed data on LOS when considering the length of stay in the hospital versus in the ICU among this population.
Time to consultation and LOS
The study completed in 2011 by Desan, Zimbrean, Weinstein, et al. revealed that the intervention group receiving weekday proactive psychiatric consultation had reduced LOS compared to the control groups that were consulted intermittently, at variable intervals [5]. Thus, a more frequent consultation service may play a role in the decrease in LOS, perhaps as a direct result of more regular psychiatric care.
A study by Sockalingam, Alzahrani, Meaney, et al. in 2016 looked at time to referral (TTR) to proactive CL care and compared TTR to LOS. Results showed that patients with a longer time to receive C-L psychiatry had a statistically significant longer hospital LOS. Mean LOS was 12 days (range 4-28 days), but data displayed that many patients with a quicker TTR had a higher number of short LOS visits (“near zero days”) as opposed to those with a slower TTR [15].
The Triplett, Carroll, Gerstenblith, et al. 2019 study discovered that the time to consult was 2.23 days for patients receiving proactive consultation versus 3.38 days for patients receiving reactive consultation (p = < 0.001). It was noted that ensuing hospital LOS was even shorter for those who attained a faster time to consult than patients with a longer time to consult [7].
The previously discussed Chavez, Caplan, McKnight, et al. review in 2021 also found that there was a moderate to large correlation (r = .70) between time to psychiatric consultation and hospital LOS (p = <0.001) [10]. Therefore, the data shows a statistically significant direct relationship between the variables- as time to consult increases, length of stay increases as well. On the other hand, the PRIME Medicine study completed in 2021 by Oldham, Lang, Hopkin, et al. did not find a statistically significant time to consultation and resulting LOS change when comparing PRIME units to the general population group (3.8 days versus 4.0 days) [11]. As previously discussed, there were many limitations to this study that must be considered.
The Triplett, Prince, Bienvenu, et al. study in 2024 also found that patients seen first by the proactive service team had a shorter time to consultation at 2.87 days as compared to 3.61 days in patients seen by the on-request service team (p = < 0.001) [12]. The patients with a faster consultation from the proactive service team did have a decrease in LOS, as reported above.
Proactive C-L psychiatry healthcare staff satisfaction
The 2019 study by Triplett, Carroll, Gerstenblith, et al. looked at nurse and physician satisfaction with proactive C-L psychiatry by asking staff to answer a pre- and post-implementation questionnaire. The staff was asked to respond to the statement “Help is available to me when I need assistance with patients who have comorbid behavioral or psychiatric issues” both before and after implementing the proactive consultation model with a full C-L team. Among the nurses surveyed, 61% responded with “somewhat agreed or strongly agree” before implementing the service, which rose to 80% afterwards. Among the physicians measured, 21% responded to the same posed statement with “somewhat agreed or strongly agree” prior to implementation, with 87% of responders stating “somewhat agreed or strongly agree” after implementation. Both of these changes were determined to be statistically significant [7]. The increase in fulfillment from these clinicians may stem from the support provided by a whole-team approach to care that proactive C-L psychiatry provides.
Decreased LOS and readmission rates
The 2022 retrospective cohort study by Lanvin, Vulser, Vinant, et al. acknowledged that previous studies had revealed a reduced LOS with proactive psychiatric consultation. However, the authors wished to explore the impact of proactive C-L psychiatry and decreased LOS on the rates of readmission in these patients. Looking at patients who had received a proactive psychiatry consult, they reported that the risk of readmission within 30 days of discharge was significantly higher in those who had a longer LOS, later time to consultation, and higher disease severity. Results stated a statistically significant mean LOS of 21.1 days among those who were not readmitted within 30 days, while the mean LOS was 27 days in 30-day readmitted patients (p = < 0.001). They also reported an average LOS of 21.7 days among patients who were not readmitted within 7 days compared to an average LOS of 25.01 days in 7-day readmitted patients (p = 0.15), which was not a statistically significant difference [16]. Therefore, this data poses the question of whether proactive C-L psychiatry and a reduced hospital LOS may lead to a lower rate of hospital readmission. While it cannot be stated as a causation, it certainly does establish a correlation between the two variables.
This review strongly supports the adoption of proactive C-L psychiatry as the preferred approach for inpatient consultation services in the adult patient population. The results of the articles analyzed in this review demonstrate a clear relationship between proactive C-L psychiatry and hospital length of stay. It can be stated that all of the studies included in the review reported a reduced LOS when a proactive psychiatric consultation service was used in comparison to a standard, on-request model of psychiatric consultation. The majority of studies applied this model to the general inpatient population, but results were applicable to ICU inpatients as well. The findings also revealed that a shorter time to obtain a psychiatric consultation led to a decreased LOS. While the data is limited on readmission rates among proactive C-L psychiatry patients, the outcomes known to date do demonstrate a lower rate of readmission. Lastly, the small sample size of research that has investigated the impact of proactive C-L psychiatry on physician, nurse, and other hospital staff satisfaction has shown increased approval.
Therefore, it can be suggested that earlier, quicker C-L psychiatry services present more benefits to hospital LOS and patient care than the standard, reactive consultation services do. However, it is important to acknowledge the limitations of this study. A relatively small sample size was included for review due to a lack of obtainable research on this topic to date, as the database search yielded a low number of eligible articles. Also, the significance of the reduction of LOS did vary among the studies included in the results— some articles reported a decreased LOS in the intervention group compared to the control group which was not statistically significant. Additionally, the articles represented a wide array of adult patient populations, hospital settings, and underlying diseases and conditions that may have contributed to the variations in LOS data.
Due to the limited amount of research on this matter, future investigations are warranted to expand our knowledge on this topic. It is also recommended that future studies aim to address additional patient populations that may benefit from proactive C-L psychiatry. There is especially a need for examination of the pediatric population, as there is a severe shortage of data pertaining to this topic in patients under the age of 18. It is also recommended to explore the impact of proactive C-L psychiatry and resultant LOS on patients without an underlying mental health disorder, as most studies use the consultation model on patients with a known mental illness or diagnosed psychiatric disorder. Additionally, while studies have started to look at healthcare staff satisfaction with the proactive service, there is little reported data on patient satisfaction with its use. More research on resultant rates of readmission is necessary as well. Nevertheless, this study marks a significant step in advancing the understanding of inpatient proactive consultation psychiatry in adults and its impact on hospital LOS.
Results of this review show a subsequent reduction in mean hospital LOS when proactive C-L psychiatry services are used compared to reactive, on-request consultation services. A shortened LOS is seen with this practice when there is a faster time for consultation or referral. The findings are applicable to general and ICU populations, and rate of readmission may be decreased in these groups. However, it is clear that further studies are necessary to determine the significance of the results, as very little research to date has been completed on the topic. It is recommended to expand the scope of investigation to more patient populations, especially those without an underlying mental health illness. It is also advisable to further investigate the service’s impact on both healthcare team and patient satisfaction. Overall, the research to date shows evidence of proactive C-L psychiatry’s success in decreasing average hospital LOS and improving patient care measures. The proactive C-L psychiatry service model demonstrates great potential to become the standard of care in the inpatient setting.
The author would like to recognize the contributions of Lauren Haley, OMS III, Jonathan Irby, OMS III, and Sydney Klumb, OMS III, as well as the mentorship and contributions provided by Johnny Cheng, DO. All authors are in affiliation with Rocky Vista University, College of Osteopathic Medicine, located at 8401 S Chambers Rd, Englewood, CO 80112.
- van Niekerk M, Walker J, Hobbs H, Magill N, Toynbee M, Steward B, et al. The prevalence of psychiatric disorders in general hospital inpatients: a systematic umbrella review. J Acad Consult Liaison Psychiatry. 2022;63(6):567-578. https://doi.org/10.1016/j.jaclp.2022.04.004
- Krautgartner M, Alexandrowicz R, Benda N, Wancata J. Need and utilization of psychiatric consultation services among general hospital inpatients. Soc Psychiatry Psychiatr Epidemiol. 2006;41(4):294-301. https://doi.org/10.1007/s00127-005-0025-z
- Pezzia C, Pugh JA, Lanham HJ, Leykum LK. Psychiatric consultation requests by inpatient medical teams: an observational study. BMC Health Serv Res. 2018;18(1):336. https://doi.org/10.1186/s12913-018-3171-1
- Oldham MA, Desan PH, Lee HB, Bourgeois JA, Shah SB, Hurley PJ, et al. Council on Consultation-Liaison Psychiatry. Proactive consultation-liaison psychiatry: American Psychiatric Association resource document. J Acad Consult Liaison Psychiatry. 2021;62(2):169-185. https://doi.org/10.1016/j.jaclp.2021.01.005
- Desan PH, Zimbrean PC, Weinstein AJ, Bozzo JE, Sledge WH. Proactive psychiatric consultation services reduce length of stay for admissions to an inpatient medical team. Psychosomatics. 2011;52(6):513-20. https://doi.org/10.1016/j.psym.2011.06.002
- Sledge WH, Gueorguieva R, Desan P, Bozzo JE, Dorset J, Lee HB. Multidisciplinary proactive psychiatric consultation service: impact on length of stay for medical inpatients. Psychother Psychosom. 2015;84(4):208-16. https://doi.org/10.1159/000379757
- Triplett P, Carroll CP, Gerstenblith TA, Bienvenu OJ. An evaluation of proactive psychiatric consults on general medical units. Gen Hosp Psychiatry. 2019;60:57-64. https://doi.org/10.1016/j.genhosppsych.2019.07.009
- Oldham MA, Chahal K, Lee HB. A systematic review of proactive psychiatric consultation on hospital length of stay. Gen Hosp Psychiatry. 2019;60:120-126. https://doi.org/10.1016/j.genhosppsych.2019.08.001
- Bronson BD, Alam A, Schwartz JE. The impact of integrated psychiatric care on hospital medicine length of stay: a pre-post intervention design with a simultaneous usual care comparison. Psychosomatics. 2019;60(6):582-590. https://doi.org/10.1016/j.psym.2019.05.004
- Chavez MA, Caplan JP, McKnight CA, Schlinkert AB, Chapple KM, Mankin JA, et al. Early psychiatric consultation is associated with decreased cost and length of stay in the patient population at a Level I trauma center. Cureus. 2021;13(8). https://doi.org/10.7759/cureus.17572
- Oldham MA, Lang VJ, Hopkin JL, Maeng DD. Proactive integration of mental health care in hospital medicine: PRIME medicine. J Acad Consult Liaison Psychiatry. 2021;62(6):606-616. Available from: https://doi.org/10.1016/j.jaclp.2021.06.005
- Triplett PT, Prince E, Bienvenu OJ, Gerstenblith A, Carroll CP. An observational study of proactive and on-request psychiatry consultation services: evidence for differing roles and outcomes. J Acad Consult Liaison Psychiatry. 2024;65(4):338-346. Available from: https://doi.org/10.1016/j.jaclp.2024.03.003
- Sharpe M, Walker J, van Niekerk M, Toynbee M, Magill N, Frost C, et al. HOME Study Team. Proactive integrated consultation-liaison psychiatry and time spent in hospital by older medical inpatients in England (The HOME Study): a multicentre, parallel-group, randomised controlled trial. Lancet Psychiatry. 2024;11(9):684-695. Available from: https://doi.org/10.1016/s2215-0366(24)00188-3
- Bui M, Thom RP, Hurwitz S, Levy-Carrick NC, O'Reilly M, Wilensky D, et al. Hospital length of stay with a proactive psychiatric consultation model in the medical intensive care unit: a prospective cohort analysis. Psychosomatics. 2019;60(3):263-270. Available from: https://doi.org/10.1016/j.psym.2018.07.011
- Sockalingam S, Alzahrani A, Meaney C, Styra R, Tan A, Hawa R, et al. Time to consultation-liaison psychiatry service referral as a predictor of length of stay. Psychosomatics. 2016;57(3):264-272. Available from: https://doi.org/10.1016/j.psym.2016.01.005
- Vulser H, Vinant V, Lanvin V, Chatellier G, Limosin F, Lemogne C. Association between the timing of consultation-liaison psychiatry interventions and the length of stay in general hospital. Br J Psychiatry. 2021;218(4):204-209. Available from: https://doi.org/10.1192/bjp.2019.233